Abstract
Background
Some patients prescribed opioid analgesic medications (OAs) for pain experience serious side-effects including dependence, sedation, and overdose. Because most patients are at low risk for OA-harms, risk reduction interventions requiring multiple conversations with a counselor are impractical on a large scale. Objective. We evaluated whether an intervention based on reinforcement learning (RL), a field of artificial intelligence, could learn through experience to personalize interactions with pain patients discharged from the emergency department (ED) and decrease OA misuse behaviors while conserving counselors’ time.
Methods
Data represent 2,439 weekly interactions between a digital health intervention (PowerED) and 228 patients with pain discharged from two EDs who reported opioid misuse in the prior three months. During each patient’s 12-weeks of intervention, PowerED used RL to select among three treatment options: a brief motivational message delivered via an Interactive Voice Response (IVR) call, a more extended motivational IVR call, or a live call from a counselor. The algorithm selected session types for each patient each week with the goal of minimizing future OA risk, defined in terms of a dynamic score reflecting patient reports during IVR monitoring calls. When a live counseling call was predicted to have a similar impact on future OA risk as an IVR message, the algorithm favored IVR to conserve counselor time. We used logit models to estimate changes in the relative frequency of each session type as PowerED gained experience. Poisson regression was used to examine changes in self-reported OA risk scores over calendar time, controlling for patients’ session number.
Results
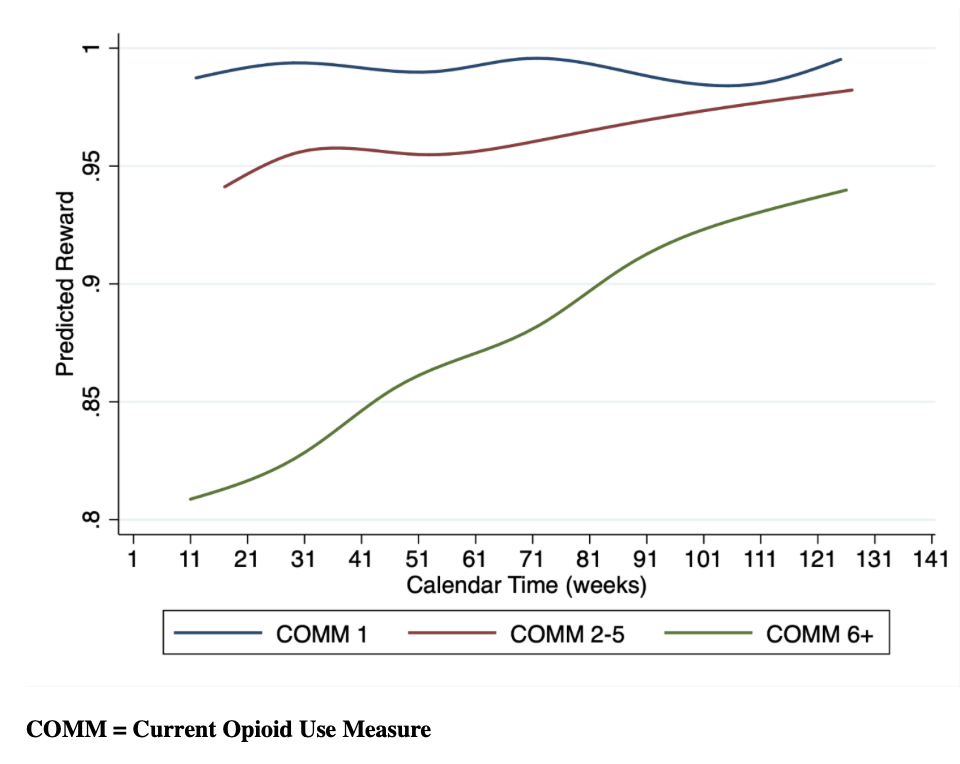
Participants were on average 40 years of age, 67% were women, and 49% were unemployed. Most participants (77%) reported chronic pain, 49% reported near daily opioid use, and 46% had moderate/severe depressive symptoms. As PowerED gained experience through interactions over a period of 142 weeks, it delivered fewer live counseling sessions relative to brief IVR sessions (P = .006) and extended IVR sessions (P < .001). Live counseling sessions were selected 33.5% of the time in the first five weeks of interactions (95% CI: 27.4%, 39.7%), but only for 16.4% of sessions (95% CI: 12.7%, 20.0%) after 125 weeks. Controlling for each patient’s changes during their course of treatment, this adaptation of treatment-type allocation led to progressively greater improvements in self-reported OA risk scores (P < .001) over calendar time, as measured by the number of weeks since enrollment began. Improvement over time in risk behaviors was especially pronounced among patients with the highest risk at baseline (P = .02).
Conclusions
This RL-supported program learned which treatment modalities worked best to improve self-reported OA risk behaviors while conserving counselors’ time. RL-supported interventions represent a scalable solution for patients with pain receiving OA prescriptions.
ClinicalTrials.Gov. NCT02990377
Keywords
Artificial intelligence, opioid safety, telehealth, reinforcement learning, pain management