Key Points
- Non-clinical factors may be associated with anticoagulant use for cancer associated thrombosis.
- We conducted a retrospective cohort study of over 12,000 patients using insurance claims data.
- ower household income was associated with warfarin use over other anticoagulants.
- Geographic region and educational attainment were also associated with anticoagulant use.
Abstract
Introduction: Cancer associated thrombosis (CAT) is a leading cause of death among patients with cancer. It is not clear if non-clinical factors are associated with anticoagulation receipt.
Methods: We conducted a retrospective cohort study of Optum’s de-identified Clinformatics Database of adults with cancer diagnosed between 2009 and 2016 who developed CAT, treated with an outpatient anticoagulant (warfarin, low molecular weight heparin, LMWH, or a direct oral anticoagulant, DOAC).
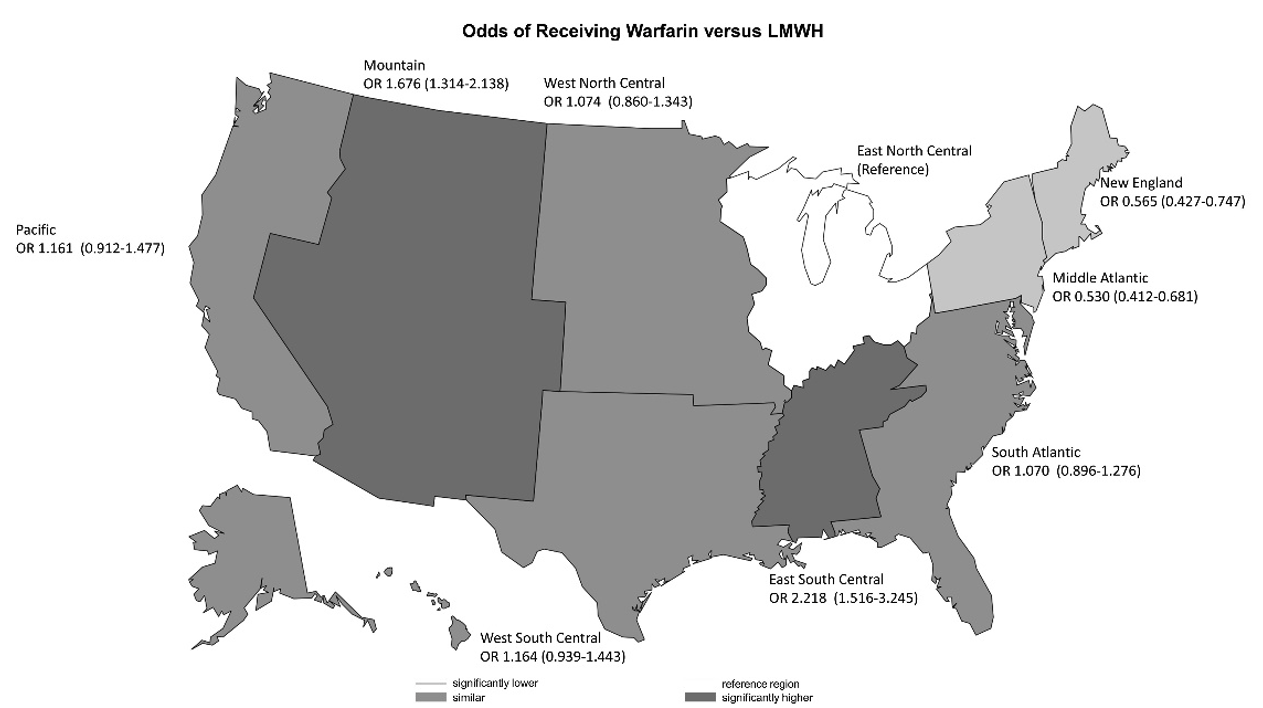
Results: Of 12,622 patients, three months after an episode of CAT, 1,485 (12%) were on LMWH, 1,546 (12%) on DOACs, and 9,591 (76%) were on warfarin. When controlling for other factors, anticoagulant use was significantly associated with socioeconomic factors, region, co-morbidities, type of thrombosis, and cancer subtype. Patients with a bachelor’s degree or greater level of education were less likely to receive warfarin (OR: 0.77; 95% CI: [0.59, 0.99]; p<0.046) or DOACs (OR: 0.67; 95% CI: [0.55, 0.82]; p<0.001) compared to LMWH. Patients with higher income levels were more likely to receive LMWH or DOACs compared to warfarin, while patients across all income levels were equally likely to receive LMWH or DOACs.