Importance: Venous thromboembolism (VTE) is a leading cause of death in patients with cancer. Inferior vena cava (IVC) filters are utilized to mitigate the risk of pulmonary embolism (PE) for patients who have contraindication to or failure of anticoagulation.
Objective: To identify predictors of IVC filter placement and retrieval in patients with cancer associated thrombosis.
Design: Retrospective cohort study from January 2012 to June 2016.
Settings: Insurance claims data from a nationally representative database. Participants: Adults with a diagnosis of cancer and receiving cancer directed therapy along with a new diagnosis of VTE were included. Patients were followed until the end of the study period or loss to follow-up.
Exposures: IVC filter placement and retrieval
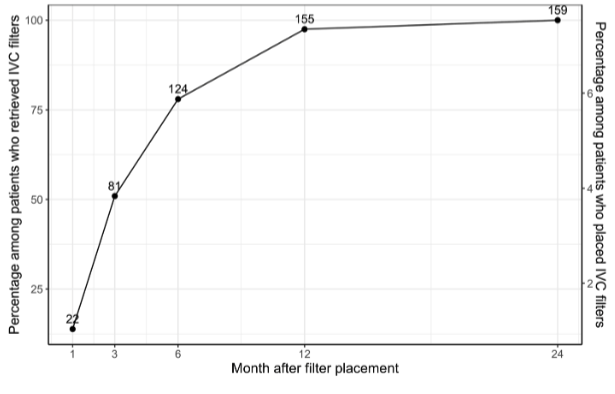
Main Outcomes: Type of venous thrombosis, type of malignancy, comorbidities, surgical history, anticoagulation use, education, household income, race, age, sex, and geographic region. Results: 25,788 patients (mean [SD] age: 68.3 [12.7] years) met the study inclusion criteria, with 2,111 individuals (8.2%) undergoing IVC filter placement. Filter placement was associated with the type of thrombosis, malignancy, recent surgery, co-morbidities, and income. A total of 137 patients (6.5%) newly started anticoagulation within 3 days of filter placement and 612 (29%) patients received anticoagulation within 30 days after IVC filter placement. Only 159 (7.5%) patients had their IVC filters retrieved during the study period, 49% of which were retrieved more than 3 months after placement. Patients with income between $75-99K (OR 2.13, P=0.012) or above $100K (OR 1.8, P=0.038) were more likely to have filter retrieval compared with those with income < $50K. Filter retrieval was also more likely in patients who did not have central nervous system or lung malignancies, those who were younger (0.69, P<0.001), or with less co-morbidities (0.73, P<0.01). Patients in the Mountain West region were less likely to have filter placement and more likely to have filter retrieval compared to other regions.
Conclusion: Less than 10% of patients with cancer associated thrombosis received IVC filters. IVC filter retrieval was low and is associated with sociodemographic factors. Efforts are needed to address disparities in IVC filter use and improve retrieval rates.
Key Points Question: What are predictors of inferior vena cava filter (IVC) placement and retrieval in patients with cancer-associated thrombosis (CAT)?
Findings: In this retrospective cohort study, type of thrombosis, malignancy, recent surgery, and degree of co-morbidity were associated with IVC filter placement. Less than 10% of patients had their IVC filters retrieved. Retrieval was associated with type of malignancy, age, and comorbidity. Income and region were significantly associated with filter placement and retrieval.
Meaning: IVC filter retrieval rates for CAT are low. Retrieval is associated with clinical and non-clinical factors, highlighting a need to address disparities in IVC filter use.