Abstract
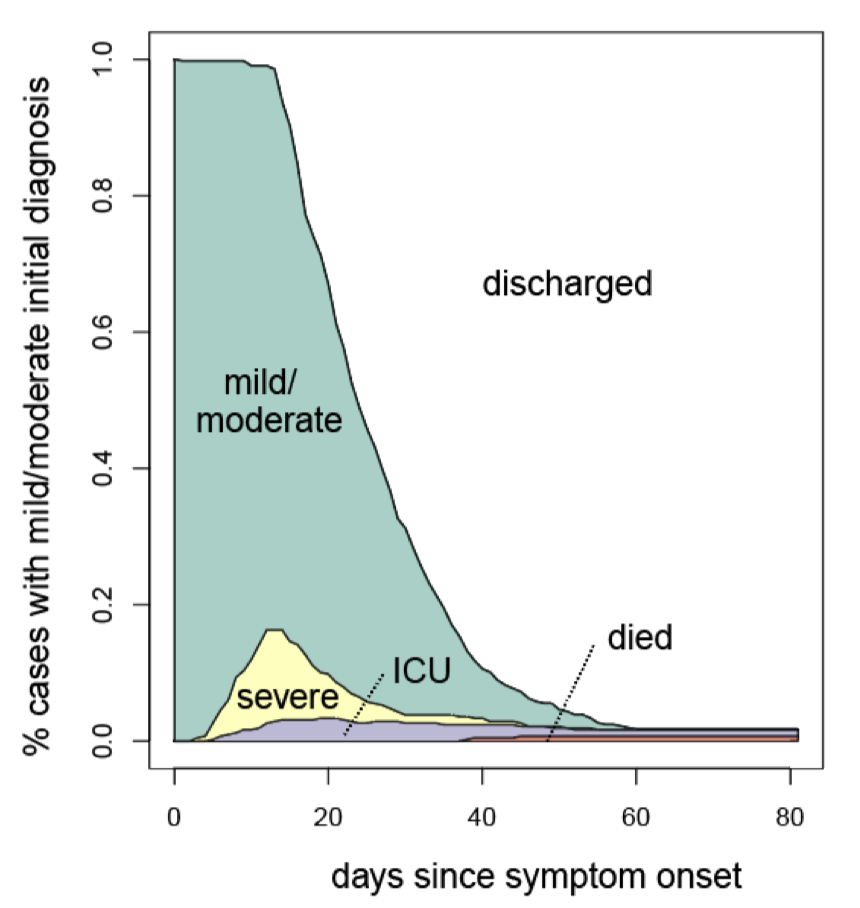
The COVID-19 pandemic has stressed healthcare care systems throughout the world. Understanding clinical progression of cases is a key public health priority that informs optimal resource allocation during an emergency. Using data from Shenzhen, China, where all cases were monitored in hospital and symptom profiles and clinical and lab results were available starting from early stages of clinical course, we characterized clinical progression of COVID-19 cases and determined important predictors for faster clinical progression to key clinical events and longer use of medical resources. Epidemiological, demographic, laboratory, clinical, and outcome data were extracted from electronic medical records. We found that those who progressed to the severe stage, developed acute respiratory distress syndrome, and were admitted to the intensive care unit (ICU) progressed on average 9.5 days (95%CI 8.7,10.3), 11.0 days (95%CI 9.7,12.3), and 10.5 days (95%CI 8.2,13.3) after symptom onset, respectively. We estimated that patients who were admitted to ICUs remained there for an average of 34.4 days (95%CI 24.1,43.2) and the average time on a ventilator was 28.5 days (95%CI 20.0,39.1) among those requiring mechanical ventilation. The median length of hospital stay was 21.3 days (95%CI, 20.5, 22.2) for the mild or moderate cases who did not progress to the severe stage, but increased to 52.1 days (95%CI, 43.3, 59.5) for those who required ICU admission. Clear characterization of clinical progression informs planning for healthcare resource allocation during COVID-19 outbreaks and provides a basis that helps assess the effectiveness of new treatment and therapeutics.