Summary
Background Pneumonia is the leading cause of death among children younger than 5 years. In this study, we estimated causes of pneumonia in young African and Asian children, using novel analytical methods applied to clinical and microbiological findings.
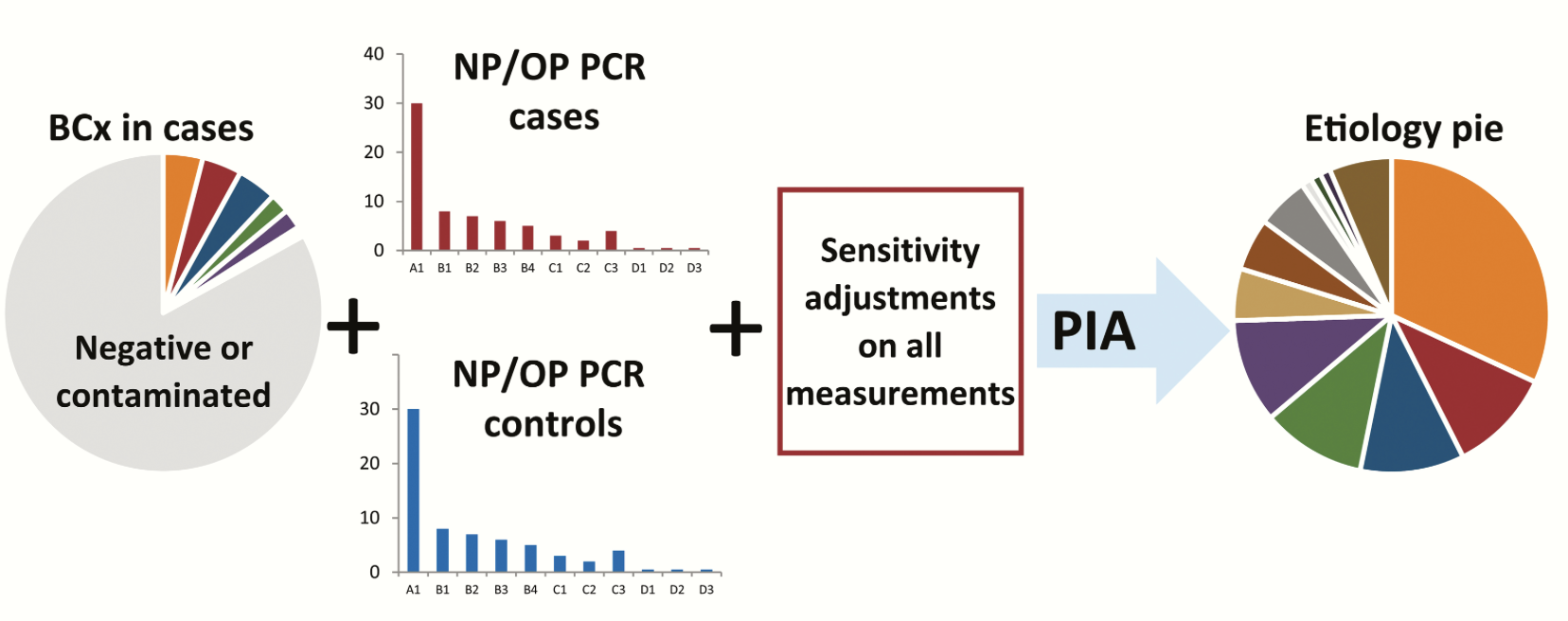
Methods We did a multi-site, international case-control study in nine study sites in seven countries: Bangladesh, The Gambia, Kenya, Mali, South Africa, Thailand, and Zambia. All sites enrolled in the study for 24 months. Cases were children aged 1–59 months admitted to hospital with severe pneumonia. Controls were age-group-matched children randomly selected from communities surrounding study sites. Nasopharyngeal and oropharyngeal (NP-OP), urine, blood, induced sputum, lung aspirate, pleural fluid, and gastric aspirates were tested with cultures, multiplex PCR, or both. Primary analyses were restricted to cases without HIV infection and with abnormal chest x-rays and to controls without HIV infection. We applied a Bayesian, partial latent class analysis to estimate probabilities of aetiological agents at the individual and population level, incorporating case and control data.
Findings Between Aug 15, 2011, and Jan 30, 2014, we enrolled 4232 cases and 5119 community controls. The primary analysis group was comprised of 1769 (41·8% of 4232) cases without HIV infection and with positive chest x-rays and 5102 (99·7% of 5119) community controls without HIV infection. Wheezing was present in 555 (31·7%) of 1752 cases (range by site 10·6–97·3%). 30-day case-fatality ratio was 6·4% (114 of 1769 cases). Blood cultures were positive in 56 (3·2%) of 1749 cases, and Streptococcus pneumoniae was the most common bacteria isolated (19 [33·9%] of 56). Almost all cases (98·9%) and controls (98·0%) had at least one pathogen detected by PCR in the NP-OP specimen. The detection of respiratory syncytial virus (RSV), parainfluenza virus, human metapneumovirus, influenza virus, S pneumoniae, Haemophilus influenzae type b (Hib), H influenzae non-type b, and Pneumocystis jirovecii in NP-OP specimens was associated with case status. The aetiology analysis estimated that viruses accounted for 61·4% (95% credible interval [CrI] 57·3–65·6) of causes, whereas bacteria accounted for 27·3% (23·3–31·6) and Mycobacterium tuberculosis for 5·9% (3·9–8·3). Viruses were less common (54·5%, 95% CrI 47·4–61·5 vs 68·0%, 62·7–72·7) and bacteria more common (33·7%, 27·2–40·8 vs 22·8%, 18·3–27·6) in very severe pneumonia cases than in severe cases. RSV had the greatest aetiological fraction (31·1%, 95% CrI 28·4–34·2) of all pathogens. Human rhinovirus, human metapneumovirus A or B, human parainfluenza virus, S pneumoniae, M tuberculosis, and H influenzae each accounted for 5% or more of the aetiological distribution. We observed differences in aetiological fraction by age for Bordetella pertussis, parainfluenza types 1 and 3, parechovirus–enterovirus, P jirovecii, RSV, rhinovirus, Staphylococcus aureus, and S pneumoniae, and differences by severity for RSV, S aureus, S pneumoniae, and parainfluenza type 3. The leading ten pathogens of each site accounted for 79% or more of the site’s aetiological fraction.
Interpretation In our study, a small set of pathogens accounted for most cases of pneumonia requiring hospital admission. Preventing and treating a subset of pathogens could substantially affect childhood pneumonia outcomes.
MeSH Key Words: pneumonia, child health, case-control studies, aetiology, developing countries